Biomedical Importance
Myoglobin and hemoglobin are vital oxygen-binding proteins that ensure efficient transport and storage of oxygen in the human body. Myoglobin, located primarily in muscles, stores oxygen for use during high metabolic demand, while hemoglobin, found in red blood cells, transports oxygen from the lungs to tissues and returns carbon dioxide to the lungs for exhalation. Alterations in these proteins lead to clinically significant conditions such as anemias, thalassemias, and myoglobinuria.
Heme & Ferrous Iron Confer the Ability to Store & Transport Oxygen
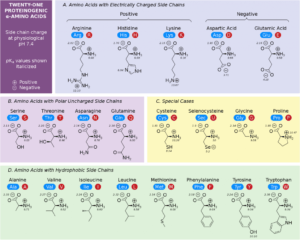
Both myoglobin and hemoglobin contain a prosthetic group called heme, which consists of a porphyrin ring with a central ferrous (Fe²⁺) iron atom. This iron atom binds reversibly to oxygen, allowing these proteins to store or transport oxygen depending on the physiological need.

Structural Features of Myoglobin
- Myoglobin Is Rich in α Helix
Myoglobin is a single-chain globular protein primarily composed of α-helical structures, which create a pocket to bind heme securely. - Histidines F8 & E7 Perform Unique Roles in Oxygen Binding
The proximal histidine (F8) coordinates directly with the iron atom, while the distal histidine (E7) stabilizes bound oxygen through hydrogen bonding, reducing the risk of oxidative damage to the iron center. - Iron Movement Toward the Plane of the Heme
When oxygen binds to myoglobin, the iron atom shifts slightly into the plane of the porphyrin ring, a movement that enhances oxygen binding. - Apomyoglobin Provides a Hindered Environment for Heme Iron
The apoprotein environment protects the heme iron from oxidation and non-specific interactions, ensuring efficient oxygen binding and release.
Oxygen Dissociation Curves for Myoglobin & Hemoglobin
The oxygen dissociation curve of myoglobin is hyperbolic, reflecting its high affinity for oxygen—ideal for oxygen storage in muscle tissues. In contrast, hemoglobin exhibits a sigmoidal (S-shaped) curve due to cooperative binding, allowing efficient oxygen loading in the lungs and unloading in tissues.

Allosteric Properties of Hemoglobins & Their Quaternary Structures
- Hemoglobin Is Tetrameric
Hemoglobin consists of four polypeptide chains (two α and two β subunits), each containing a heme group. This quaternary structure allows cooperative binding of oxygen. - Structural Similarities Between Myoglobin & Hemoglobin Subunits
Each subunit of hemoglobin resembles myoglobin in its secondary and tertiary structure, but hemoglobin’s quaternary arrangement gives it unique regulatory properties. - Oxygenation Triggers Conformational Changes
Binding of oxygen to one subunit shifts hemoglobin from the tense (T) state to the relaxed (R) state, increasing the affinity of remaining subunits for oxygen. - P50 Reflects Oxygen Affinity
The partial pressure of oxygen at which hemoglobin is 50% saturated (P50) is a key parameter that distinguishes hemoglobins with different oxygen affinities.
Transport of CO₂ and Protons
After releasing oxygen at the tissues, hemoglobin binds carbon dioxide and protons for transport back to the lungs. Protons arise from the rupture of salt bonds when oxygen binds, while CO₂ is partly carried as carbaminohemoglobin.
Role of 2,3-Bisphosphoglycerate (BPG)
BPG stabilizes hemoglobin in the T state (low-affinity form), facilitating oxygen release to tissues under conditions of high metabolic demand.
Mutant Hemoglobins
- Methemoglobin & Hemoglobin M
These forms result from oxidation of iron to the ferric (Fe³⁺) state, which cannot bind oxygen effectively. - Hemoglobin S
A single amino acid substitution in the β-chain leads to sickle cell anemia, causing hemoglobin to polymerize under low oxygen conditions.
Biomedical Implications
- Myoglobinuria: Presence of myoglobin in urine, often due to muscle injury, can lead to kidney damage.
- Anemias: Reduced hemoglobin concentration or impaired oxygen transport leads to tissue hypoxia.
- Thalassemias: Genetic disorders causing decreased synthesis of hemoglobin subunits.
- Glycosylated Hemoglobin (HbA1c): Hemoglobin bound to glucose, used as a marker for long-term blood glucose control in diabetic patients.
SUMMARY
- Myoglobin is monomeric; hemoglobin is a tetramer of two subunit types (α2β2 in HbA). Despite having different primary structures, myoglobin and the subunits of hemoglobin have nearly identical secondary and tertiary structures.
- Heme, an essentially planar, slightly puckered, cyclic tetrapyrrole, has a central Fe²⁺ linked to all four nitrogen atoms of the heme, to histidine F8, and, in oxyMb and oxyHb, also to O₂.
- The O₂-binding curve for myoglobin is hyperbolic, but for hemoglobin it is sigmoidal, a consequence of cooperative interactions in the tetramer. Cooperativity maximizes the ability of hemoglobin both to load O₂ at the PO₂ of the lungs and to deliver O₂ at the PO₂ of the tissues.
- Relative affinities of different hemoglobins for oxygen are expressed as P50, the PO2 that half-saturates them with O2. Hemoglobins saturate at the partial pressures of their respective respiratory organs, e.g., the lung or placenta.
- On oxygenation of hemoglobin, the iron, histidine F8, and linked residues move toward the heme ring. Conformational changes that accompany oxygenation include rupture of salt bonds and loosening of quaternary structure, facilitating binding of additional O₂.
- 2,3-Bisphosphoglycerate (BPG) in the central cavity of deoxyHb forms salt bonds with the β subunits that stabilize deoxyHb. On oxygenation, the central cavity contracts, BPG is extruded, and the quaternary structure loosens.
- Hemoglobin also functions in CO₂ and proton transport from tissues to lungs. Release of O₂ from oxyHb at the tissues is accompanied by uptake of protons due to lowering of the pKa of histidine residues.
- In sickle cell hemoglobin (HbS), Val replaces the β6 Glu of HbA, creating a “sticky patch” that has a complement on deoxyHb (but not on oxyHb). DeoxyHbS polymerizes at low O₂ concentrations.
forming fibers that distort erythrocytes into sickle shapes. - Alpha and beta thalassemias are anemias that result from reduced production of α and β subunits of HbA, respectively.