The Dynamic Nature of Bone: Beyond Rigidity
Biological Activity:
Connective Tissue: Bone is classified as a connective tissue, emphasizing its role in providing structural support and connectivity within the body.
Cellular Components: Bone is not merely a static structure. It houses bone cells that play active roles in its maintenance and function. The main types of bone cells include osteoblasts, osteocytes, and osteoclasts.
Skeletal System Support:
Structural Framework: Bones serve as the framework that gives shape and form to the body.
Support and Movement: They provide a scaffold for muscles and support body movement.
Protection of Internal Organs:
Vital Organs: Bones act as protective shields for internal organs, safeguarding delicate structures like the brain and organs within the thoracic and abdominal cavities.
Mineral Balance:
Calcium Homeostasis: Bones store minerals, particularly calcium and phosphorus, contributing to the body’s mineral balance.
Dynamic Exchange: Bone tissue undergoes constant remodeling, with minerals being deposited and withdrawn based on the body’s needs.
Composition:
- Extracellular Matrix:
- Collagen and Minerals: Bone matrix comprises collagen fibers, providing flexibility, and minerals (hydroxyapatite crystals), contributing to hardness.
- Dynamic Remodeling: Continuous remodeling involves the breakdown and rebuilding of the matrix.
- Bone Cells:
- Osteoblasts: Responsible for bone formation by synthesizing the matrix.
- Osteocytes: Mature bone cells embedded in the matrix, participating in nutrient exchange and signaling.
- Osteoclasts: Involved in bone resorption, breaking down matrix components.
Physiological Balance:
- Calcium Regulation: Bones act as a reservoir for calcium, releasing or absorbing it based on physiological demands.
- Blood Cell Formation: In the bone marrow, hematopoiesis occurs, contributing to the production of blood cells.
Osteoblasts: Architects of Bone Formation
1. Introduction:
- Percentage in Bone Cells: Osteoblasts constitute a significant portion, approximately 4-6%, of all bone cells, emphasizing their crucial role in bone dynamics.
2. Origin and Precursors:
- Derivation: Osteoblasts are derived from osteoprogenitor or osteogenic cells, originating from pluripotent mesenchymal stem cells (MSCs) present in the bone marrow.
3. Location and Activity:
- Preferred Areas: Osteoblasts are primarily situated in growing areas of bone, including the endosteum and periosteum.
- Non-Divisional: Unlike some cells, osteoblasts do not undergo division, emphasizing their specialized functions.
4. Functions of Osteoblasts:
- Extracellular Matrix Synthesis:
- Structural Macromolecules: Osteoblasts play a central role in synthesizing components of the bone’s extracellular matrix, including structural macromolecules such as type I collagen, essential for bone strength.
- Proteoglycans and Proteins: Various proteoglycans and proteins contribute to the organic matrix formation.
- Bone Mineralization:
- Involvement: Osteoblasts actively participate in the mineralization of the bone matrix, a critical step for bone density and hardness.
5. Fate of Osteoblasts:
- Osteocytes and Bone Lining Cells:
- Transformation: Some osteoblasts become trapped in the bone matrix, transforming into osteocytes—cells embedded within the bone responsible for nutrient exchange and signaling.
- Bone Lining Cells: Others transition into bone lining cells, covering bone surfaces.
- Apoptosis:
- Programmed Cell Death: Remaining osteoblasts undergo programmed cell death, known as apoptosis, as part of the natural life cycle.
6. Bone Matrix Formation:
- Two-Step Process:
- Organic Matrix Formation: Osteoblasts release substances like collagen proteins and proteoglycans to create the initial organic matrix.
- Mineralization: Subsequently, they contribute to the mineralization of the matrix, imparting strength and rigidity to the bone.
Conclusion: Osteoblasts, derived from mesenchymal stem cells, emerge as key players in bone formation. Their functions extend from synthesizing the bone matrix’s organic components to actively participating in mineralization. The fate of osteoblasts diversifies, contributing to the dynamic nature of bone tissue.
Osteoclasts: The Dynamic Bone Resorbers
Cellular Structure:
- Multinucleated Cells: Osteoclasts are characterized by having multiple nuclei, often numerous, which distinguishes them from other bone cells.
- Large Size: They are relatively large cells compared to other bone cells, reflecting their role in bone resorption.
Origin and Development:
- Hematopoietic Origin: Osteoclasts originate from the hematopoietic stem cell lineage, emphasizing their role in bone tissue maintenance and repair.
- Recruitment and Fusion:
- Osteoclasts undergo a process of recruitment from precursor cells, often monocytes or macrophages.
- Fusion of these precursor cells forms the large, multinucleated osteoclasts.
Bone Resorption:
- Enzymatic Activity:
- Osteoclasts secrete enzymes, particularly acid proteases, that dissolve the mineralized matrix of bone.
- Acidification of the resorption lacuna aids in demineralization.
- Matrix and Mineral Resorption:
- The primary function is to resorb old or damaged bone tissue.
- Resorption involves breaking down both the organic matrix (collagen, proteoglycans) and the mineralized components of bone.
Role in Bone Remodeling:
- Remodeling and Repair:
- Essential for the ongoing process of bone remodeling, where old bone is replaced by new bone.
- Crucial in bone repair after injury or micro-damage.
- Mineral Balance:
- Contributes to maintaining the balance of minerals in bone tissue.
Regulation:
- Cell Signaling:
- Osteoclast activity is regulated by signaling molecules, including cytokines and growth factors.
- Interaction with Osteoblasts:
- Coordination with osteoblasts: Osteoclasts and osteoblasts work in concert to maintain bone homeostasis.
Conclusion: Osteoclasts play a pivotal role in the dynamic process of bone remodeling by resorbing old or damaged bone tissue. Their multinucleated structure and origin from hematopoietic stem cells highlight their unique contributions to the maintenance and repair of the skeletal system. The interplay between osteoclasts and other bone cells ensures the continuous renewal and adaptation of bone tissue.
Osteocytes: The Guardians of Bone Integrity
Cellular Structure:
- Mature Bone Cells: Osteocytes represent the mature, fully differentiated form of bone cells.
- Location and Abundance:
- Found in lacunae, small cavities within the bone matrix.
- Constitute the majority, approximately 90-95%, of cells in mature adult bone tissue.
Origin and Development:
- Derivation from Osteoblasts:
- Osteocytes originate from osteoblasts, the bone-forming cells.
- Formation occurs when osteoblasts become surrounded and entrapped by the mineralized matrix they secrete during bone formation.
- Lifespan and Division:
- Possess a prolonged lifespan, estimated to be up to 25 years.
- Unlike osteoblasts, osteocytes do not undergo cell division.
Roles and Functions:
- Bone Preservation:
- Contribute to the maintenance and preservation of the mineral composition of bone tissue.
- Bone Deposition:
- Can deposit bone matrix, particularly in response to mechanical stresses or micro-damage.
- Communication and Signaling:
- Play a crucial role in signaling other osteocytes and bone cells about damage or changes in the bone environment.
- Regulation of Bone Cell Activities:
- Regulate the activities of osteoblasts (bone-forming) and osteoclasts (bone-resorbing).
Cellular Communication:
- Canaliculi:
- Osteocytes communicate with each other and with cells on the bone surface through long channels called canaliculi.
- These canaliculi also serve for the exchange of nutrients and waste products.
Integration in Bone Tissue:
- Network Formation:
- Osteocytes form a network within the bone matrix, creating a coordinated and integrated system.
- Mechanosensing:
- Sensing mechanical forces: Osteocytes can detect mechanical strains and contribute to bone adaptation.
Conclusion: Osteocytes, residing within the lacunae of bone tissue, play a pivotal role in maintaining bone integrity, responding to mechanical stresses, and orchestrating the activities of other bone cells. Their extensive network and communication through canaliculi underscore their significance in the dynamic processes of bone homeostasis and adaptation.
Structure of Bone: An Intricate Framework
Composition of Bone:
- Connective Tissue:
- Bones are complex connective tissues consisting of bone cells and an extracellular matrix.
- Matrix Components:
- Approximately 60% inorganic components, including hydroxyapatite crystals for hardness.
- 30% organic components, primarily collagen, along with proteoglycans and non-collagenous proteins.
- 10% water.
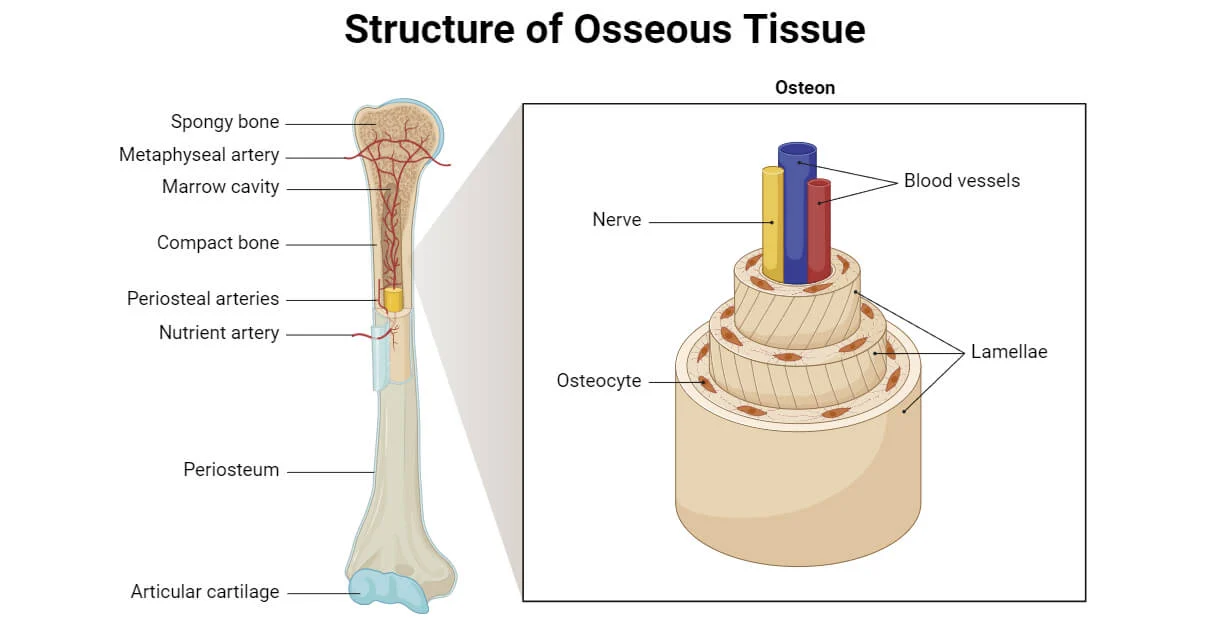
Types of Bone Tissues:
- Cortical (Compact) Bone:
- Outer shell providing shape, strength, and protection.
- Contains cylindrical osteons or Haversian systems with concentric lamellae, nerves, and blood vessels.
- Cancellous (Trabecular or Spongy) Bone:
- Porous and highly vascular internal tissue beneath compact bone.
- Supports mineral exchange, maintains skeletal strength, and contains spaces filled with bone marrow.
Structural Features:
- Compact Bone:
- Forms the outer layer and surrounds spongy bone.
- Osteons/Haversian systems with concentric lamellae contribute to its structural integrity.
- Provides shape, strength, and protection to bones.
- Spongy Bone:
- Porous and highly vascular.
- Supports mineral exchange, maintains skeletal strength, and contains bone marrow-filled spaces.
Tissue Layers:
- Periosteum:
- Outermost tissue layer covering the external surface of cortical bone.
- Contains osteoprogenitor cells.
- Involved in bone development and repair.
- Endosteum:
- Inner tissue layer lining the inner spongy bone.
- Contains osteoprogenitor cells.
- Participates in bone development and repair.
Conclusion: The intricate structure of bone, comprising cortical and cancellous tissues, reflects a dynamic framework. The matrix composition, along with the organization of compact and spongy bone, ensures the strength, support, and functionality of the skeletal system. Periosteum and endosteum, enriched with osteoprogenitor cells, contribute to the continuous processes of bone development and repair.
Structure of Bone Cells: A Cellular Symphony in Skeletal Function
1. Osteoblasts: Architects of Bone Formation
- Location: Found on bone surfaces actively engaged in formation.
- Morphology: Cuboidal or columnar cells.
- Features: Abundant rough endoplasmic reticulum and prominent Golgi apparatus, indicative of active protein synthesis.
2. Osteoclasts: Demolition Crew with Specialized Features
- Nuclei: Multinucleated cells derived from precursor cell fusion.
- Ruffled Border: Unique structure enriched with enzymes for breaking down bone minerals and matrix.
- Clear Zone: Creates an acidic microenvironment crucial for bone resorption.
3. Osteocytes: The Sentinels of Skeletal Maintenance
- Maturity: Derived from osteoblasts, representing mature bone cells.
- Morphology: Flat and almond-shaped.
- Cellular Components: Reduced Golgi complex and rough endoplasmic reticulum.
- Extensions: Project long, hair-like dendrites into canaliculi, forming an intricate network.
Conclusion: The diverse structures of osteoblasts, osteoclasts, and osteocytes contribute to the dynamic processes of bone formation, resorption, and maintenance. Osteoblasts, with their protein synthesis machinery, sculpt new bone; osteoclasts, with unique features, play a vital role in bone breakdown; while osteocytes, strategically positioned, monitor and communicate within the bone matrix, ensuring its health and equilibrium. Together, these cells orchestrate the continuous symphony of skeletal function.
Functions of Bone Cells: Masters of Skeletal Symphony
1. Osteoblasts: Architects of Bone Formation
- Bone Matrix Synthesis: Major contributors to bone formation, synthesizing the bone matrix for structural integrity.
- Organic Components: Produce essential components, including collagen, shaping the organic framework of bone.
- Mineral Deposition: Promote the deposition of minerals, such as calcium, contributing to bone hardness.
2. Osteoclasts: Dynamic Bone Remodelers
- Bone Resorption: Key players in bone remodeling, responsible for breaking down bone tissue.
- Mineral Release: Release minerals like calcium and phosphate into the bloodstream, supporting metabolic needs.
3. Osteocytes: Sentinels of Bone Health
- Mechanical Sensing: Sense mechanical stresses on bones, contributing to the adaptation of bone tissue.
- Nutrient Exchange: Facilitate the exchange of nutrients and waste products through their intricate network of canaliculi.
- Regulatory Role: Control activities of osteoblasts and osteoclasts, maintaining bone homeostasis.
- Endocrine Regulation: Act as endocrine regulators of phosphate metabolism, influencing systemic processes.
Conclusion: In the orchestration of skeletal function, osteoblasts, osteoclasts, and osteocytes play distinct yet interconnected roles. Osteoblasts sculpt and fortify bone, osteoclasts remodel and release vital minerals, while osteocytes act as vigilant regulators, sensing stresses and maintaining the delicate balance of bone metabolism. Together, these cells form a symphony of functions, ensuring the dynamic health and functionality of the skeletal system.
Bone Remodeling: The Art of Continuous Transformation
1. Dynamic Nature of Bones:
- Constant Change: Bones are not static; they undergo continuous remodeling throughout life.
- Adaptation: Remodeling allows bones to adapt to mechanical stresses and repair damage.
2. Bone Remodeling Process:
- Multicellular Units: Orchestrated by Bone Multicellular Units (BMUs) consisting of osteoblasts and osteoclasts.
- Sequential Phases:
- Activation Phase: Osteoclasts recruited to targeted areas.
- Resorption Phase: Osteoclasts break down or resorb old or damaged bone tissue.
- Reversal Phase: Osteoclasts undergo apoptosis, paving the way for osteoblasts.
- Formation Phase: Osteoblasts synthesize a new bone matrix that mineralizes, completing the cycle.
3. Purpose and Benefits:
- Mature Structure: Contributes to the development and maintenance of the mature bone structure.
- Calcium Regulation: Regulates calcium levels in the body by releasing minerals during resorption.
4. Role of BMUs:
- Coordination: BMUs coordinate the sequential actions of bone-resorbing osteoclasts and bone-forming osteoblasts.
- Harmony: Ensures a harmonious balance between bone removal and formation.
Conclusion: Bone remodeling is an intricate dance of cellular activity, ensuring that bones remain robust, adaptable, and responsive to the ever-changing needs of the body. Orchestrated by BMUs, this continuous process is vital for maintaining skeletal integrity, adapting to challenges, and regulating essential minerals, ultimately contributing to the dynamic harmony of the skeletal system.
Diseases and Disorders of Bone Cells: Unraveling the Skeletal Challenges
1. Osteoporosis:
- Characteristics: Reduced bone density and mass, increased susceptibility to fractures.
- Cause: Imbalance between bone resorption and formation, often linked to aging, hormonal changes, or nutritional deficiencies.
- Impact: Fragile bones, increased fracture risk.

2. Osteogenesis Imperfecta:
- Characteristics: Genetic disorder causing brittle bones, often known as “brittle bone disease.”
- Cause: Mutation in collagen production, affecting bone strength.
- Impact: Fragile bones, frequent fractures.
3. Rickets:
- Characteristics: Softening and weakening of bones, often in children.
- Cause: Vitamin D deficiency, inadequate calcium or phosphorus intake.
- Impact: Bowing of legs, delayed growth.
4. Paget’s Disease:
- Characteristics: Excessive bone breakdown and formation, leading to abnormal bone structure.
- Cause: Genetic factors, viral infection.
- Impact: Enlarged and deformed bones, pain.
5. Achondroplasia:
- Characteristics: Dwarfism, disproportionately short limbs.
- Cause: Genetic mutation affecting cartilage formation.
- Impact: Short stature, joint problems.
6. Osteomalacia:
- Characteristics: Softening of bones in adults.
- Cause: Vitamin D deficiency, malabsorption issues.
- Impact: Bone pain, muscle weakness.
7. Fibrous Dysplasia:
- Characteristics: Abnormal development of fibrous tissue in place of bone.
- Cause: Genetic mutations.
- Impact: Weakened bones, deformities.
8. Marfan Syndrome:
- Characteristics: Connective tissue disorder affecting bones, joints, and other systems.
- Cause: Genetic mutation in fibrillin gene.
- Impact: Tall stature, joint issues.
Conclusion: Diseases and disorders affecting bone cells highlight the intricate interplay of genetics, nutrition, and hormonal balance in maintaining skeletal health. Understanding these conditions is crucial for diagnosis, treatment, and ongoing research to enhance bone health and overall well-being.