Blood clotting (Clotting Factors), or coagulation, is a vital process that prevents excessive bleeding when a blood vessel is injured. The coagulation system involves a complex cascade of events, primarily orchestrated by a group of proteins known as clotting factors. These factors work together to form a stable blood clot, which seals wounds and initiates the healing process. In this article, we’ll explore the various clotting factors, their functions, and their significance in maintaining hemostasis.
What are Clotting Factors? (List)
Clotting factors are proteins found in blood plasma that play a critical role in the coagulation process. They are generally designated by Roman numerals (I through XIII), and each factor has a specific role in the clotting cascade. When activated, these factors interact in a precise sequence, leading to the formation of a fibrin clot. Let’s delve into the key clotting factors and their functions:
| Clotting Factor (in numeral form) | Clotting Factor (name) | Functions |
| Factor I | Fibrinogen | The precursor to fibrin, which forms the structural basis of a blood clot. |
| Factor II | Prothrombin | Converted to thrombin, which then transforms fibrinogen into fibrin. ; Activates platelets and clotting factors I, V, VII, VIII, XI, XIII, etc. during the clotting process |
| Factor III | Thromboplastin (Tissue factor) | Initiates the extrinsic pathway of coagulation. ; Initiation of thrombin formation |
| Factor IV | Calcium Ion | Essential for various steps in the coagulation cascade. ; Initiates and regulates the binding of coagulation factors and phospholipids and acts as a cofactor of several other clotting factors |
| Factor V | Proaccelerin (Labile factor) | Acts as a cofactor in the conversion of prothrombin to thrombin. ; Co-factor of factor X |
| Factor VII | Proconvertin (Stable factor) | Activates Factor X in the extrinsic pathway. ; Promote the formation of prothrombin conversion into thrombin Activate factor IX and factor X |
| Factor VIII | Antihemophilic factor A | Works with Factor IX to activate Factor X in the intrinsic pathway. ; Combine with factor IXa and accelerate the activation of factor X by IXa |
| Factor IX | Antihemophilic factor B(Plasma thromboplastin)(Christmas factor) | Part of the intrinsic pathway, activating Factor X. ; Activate the factor X |
| Factor X | Stuart-Prower factor | Converts prothrombin to thrombin in the common pathway. ; Form prothrombinase complex Activate factor II |
| Factor XI | Antihemophilic factor C (Plasma Thromboplastin Antecedent) | Activates Factor IX in the intrinsic pathway. ; Co-factor of factor IX and activate it |
| Factor XII | Hageman factor | Initiates the intrinsic pathway by activating Factor XI. ; Activate factor VII, factor XI, plasminogen |
| Factor XIII | Fibrin stabilizing factor (Laki-Lorand factor) | Stabilizes the fibrin clot by cross-linking fibrin strands. ; Promotes crosslinking of fibrin fibers |
Accessory clotting factors
“Fitzgerald” and “Fletcher” refer to specific deficiencies associated with the proteins HMWK (High-Molecular-Weight Kininogen) and Prekallikrein, respectively, in the context of the coagulation cascade:
- Fitzgerald Trait (Fitzgerald Factor):
- Description: This refers to a deficiency of High-Molecular-Weight Kininogen (HMWK). HMWK, also known as Fitzgerald factor, is essential in the intrinsic pathway of the coagulation cascade. It acts as a cofactor in the activation of prekallikrein and Factor XI by Factor XIIa.
- Clinical Presentation: Despite the deficiency, individuals with Fitzgerald trait typically do not experience bleeding disorders. This is because HMWK is not directly involved in forming blood clots but rather in facilitating the activation of other factors. However, laboratory tests may show a prolonged activated partial thromboplastin time (aPTT).
- Fletcher Trait (Fletcher Factor):
- Description: This refers to a deficiency of Prekallikrein, which is also known as Fletcher factor. Prekallikrein, when activated to kallikrein, plays a role in the intrinsic pathway of blood coagulation by activating Factor XII and contributing to the activation of Factor XI.
- Clinical Presentation: Similar to Fitzgerald trait, individuals with Fletcher trait usually do not exhibit bleeding problems, even though they have a prolonged aPTT. The intrinsic coagulation pathway can be initiated through alternate routes, compensating for the lack of prekallikrein.
Both Fitzgerald and Fletcher deficiencies highlight the redundancy and complexity of the coagulation cascade, where multiple pathways and factors ensure that the blood clotting process can still function effectively even when certain components are deficient.
Importance of Clotting Factors
Proper functioning of clotting factors is crucial for hemostasis. Deficiencies or abnormalities in these factors can lead to bleeding disorders. For instance:
- Hemophilia A: Caused by a deficiency in Factor VIII.
- Hemophilia B: Caused by a deficiency in Factor IX.
- Von Willebrand Disease: Involves a deficiency or dysfunction of von Willebrand factor, which stabilizes Factor VIII.
Stages of Hemostasis
Vascular Spasm
Immediately after a blood vessel is injured, the vessel constricts in a process called vascular spasm. This vasoconstriction reduces blood flow to the area, minimizing blood loss. The spasm is triggered by:
- Direct injury to vascular smooth muscle
- Chemicals released by endothelial cells and platelets
- Reflexes initiated by local pain receptors
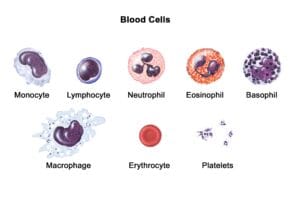
Platelet Plug Formation
Platelets adhere to the exposed collagen fibers of the damaged vessel. Once they adhere, they become activated and release chemicals that make nearby platelets sticky, forming a platelet plug. This is a temporary seal to cover the break in the vessel wall. Key substances involved in this process include:
- Adenosine diphosphate (ADP): Attracts more platelets to the site.
- Thromboxane A2: Enhances platelet aggregation and vasoconstriction.
- Serotonin: Also promotes vasoconstriction.

Coagulation (Clotting)
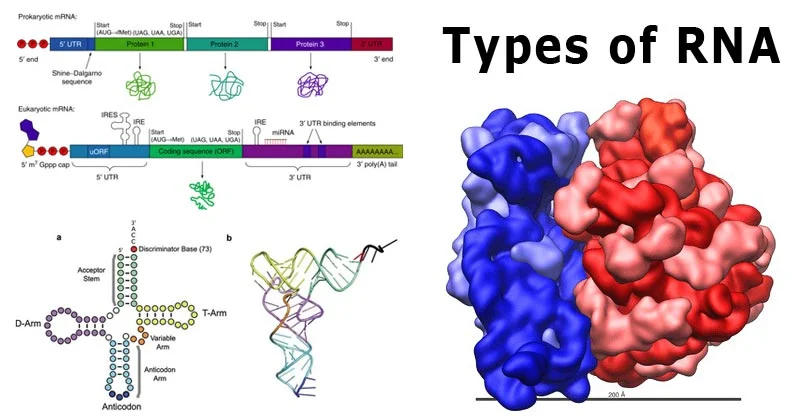
Coagulation reinforces the platelet plug with fibrin threads, creating a stable blood clot. This process involves a series of steps known as the coagulation cascade, which is divided into three pathways:

Coagulation Pathways:
- The Extrinsic Pathway (Tissue Factor Pathway):
- Triggered by external trauma that causes blood to escape from the vascular system.
- Activated by tissue factor (Factor III), which is released by damaged tissues.
- Factor VII activates Factor X in the common pathway.
- The Intrinsic Pathway (Contact Activation Pathway):
- Initiated by damage to the endothelial cells or exposure of blood to a foreign surface.
- Involves Factors XII, XI, IX, and VIII.
- Activates Factor X in the common pathway.
- The Common Pathway:
- Convergence point for both intrinsic and extrinsic pathways.
- Activation of Factor X leads to the conversion of prothrombin (Factor II) to thrombin.
- Thrombin then converts fibrinogen (Factor I) into fibrin, forming a stable clot.
- Factor XIII stabilizes the clot by cross-linking fibrin threads.

Fibrinolysis
Once the vessel is healed, the clot is no longer needed and is removed through fibrinolysis. Plasminogen, incorporated into the clot, is activated to plasmin by tissue plasminogen activator (tPA). Plasmin digests fibrin, breaking down the clot and restoring normal blood flow.
Significance of Hemostasis
Hemostasis is crucial for survival. It prevents excessive bleeding, maintains blood volume and pressure, and ensures that tissues receive adequate oxygen and nutrients. Abnormalities in hemostasis can lead to either excessive bleeding (hemorrhage) or excessive clotting (thrombosis), both of which can be life-threatening. Understanding hemostasis is vital for diagnosing and treating bleeding disorders, managing surgical patients, and developing anticoagulant therapies.