Mucosa, also known as mucous membrane, is a specialized type of epithelial tissue that lines various organs and body cavities, forming a protective layer. It is found in areas of the body that are exposed to the external environment or have openings to the outside.
Here are some key points about mucosa:
- Location:
- Mucosa lines the internal surfaces of various organs and body cavities, including the gastrointestinal tract, respiratory system, urinary tract, and reproductive organs.
- Protective Function:
- One of its primary functions is to provide a protective barrier for the underlying tissues and organs. It helps prevent infections, injuries, and dehydration.
- Orifices and Openings:
- Mucosa is present in orifices such as nostrils, ears, lips, urethral opening, anus, and other areas where the body is in contact with the external environment.
- Secretion of Mucus:
- Mucosa is associated with the secretion of mucus, a viscous and slippery fluid. Mucus is composed of water, electrolytes, proteins, and mucins (glycoproteins). Mucins are produced by specialized mucus-secreting cells called goblet cells.
- Lubrication and Protection:
- The mucus produced by mucosa serves several important functions, including lubricating surfaces, trapping and eliminating foreign particles, and protecting against microbial invasion.
- Variations in Thickness:
- The thickness of mucosa can vary depending on its location in the body. For example, the mucosa in the digestive tract is thicker and more complex than in the respiratory tract.
- Epithelial Layers:
- Mucosa typically consists of an epithelial layer, a connective tissue layer (lamina propria), and sometimes a smooth muscle layer. The type and arrangement of these layers can vary based on the specific function and location of the mucosa.
Overall, mucosa plays a vital role in maintaining the health and proper functioning of various body systems by providing a protective barrier, facilitating absorption and secretion, and contributing to the body’s defense mechanisms.
Structure of Mucous Membrane
The structure of mucous membranes, also known as mucosa, involves several layers of cells and tissues. While there can be variations in specific locations throughout the body, a general configuration applies to most mucosal membranes. The typical structure consists of three basic sub-layers:
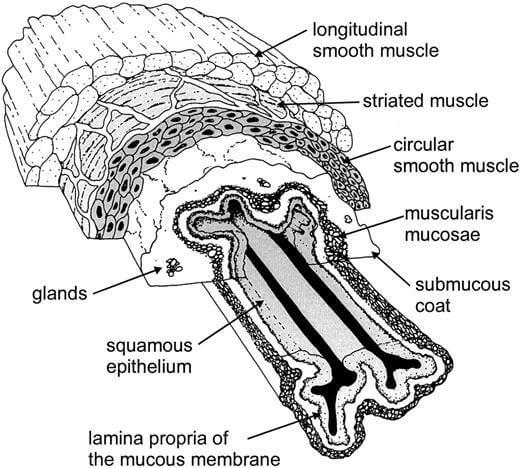
Epithelial Layer (Epithelium):
- The epithelial layer is the outermost layer of the mucous membrane, directly exposed to the external environment or the internal cavity of an organ. This layer serves as a protective barrier and is adapted to specific functions based on the location.
- The type of epithelial tissue varies, with common types including stratified squamous epithelium in areas subject to abrasion (e.g., oral cavity, esophagus), simple columnar epithelium in the digestive tract, and pseudostratified ciliated columnar epithelium in the respiratory tract.
- Specialized cells within the epithelium, such as goblet cells, contribute to the production and secretion of mucus.
Lamina Propria (Connective Tissue Layer):
- The lamina propria is a connective tissue layer located beneath the epithelium. It provides structural support and contains blood vessels, lymphatic vessels, and various immune cells. The blood vessels in this layer facilitate nutrient exchange and immune responses.
- In addition to its supportive role, the lamina propria often houses glands, blood vessels, and a network of nerve endings that contribute to the overall function of the mucous membrane.
Muscularis Mucosae (Smooth Muscle Layer):
- The muscularis mucosae is a thin layer of smooth muscle located beneath the lamina propria. This layer plays a role in the movement and function of the mucosa, aiding in processes such as the secretion of mucus and the movement of food along the digestive tract.
- While not present in all mucosal membranes, the muscularis mucosae is particularly prominent in areas with specific functional requirements, such as the gastrointestinal tract.
This three-layered structure provides mucous membranes with their characteristic properties of protection, secretion, and selective permeability. The variations in epithelial type, presence of glands, and muscularis mucosae thickness contribute to the specific functions of mucous membranes in different parts of the body.
Locations Mucous Membrane
Mucous membranes, or mucosa, line various body cavities, providing a protective layer and serving specific functions in different regions of the body. Some of the major body cavities lined by mucous membranes include:
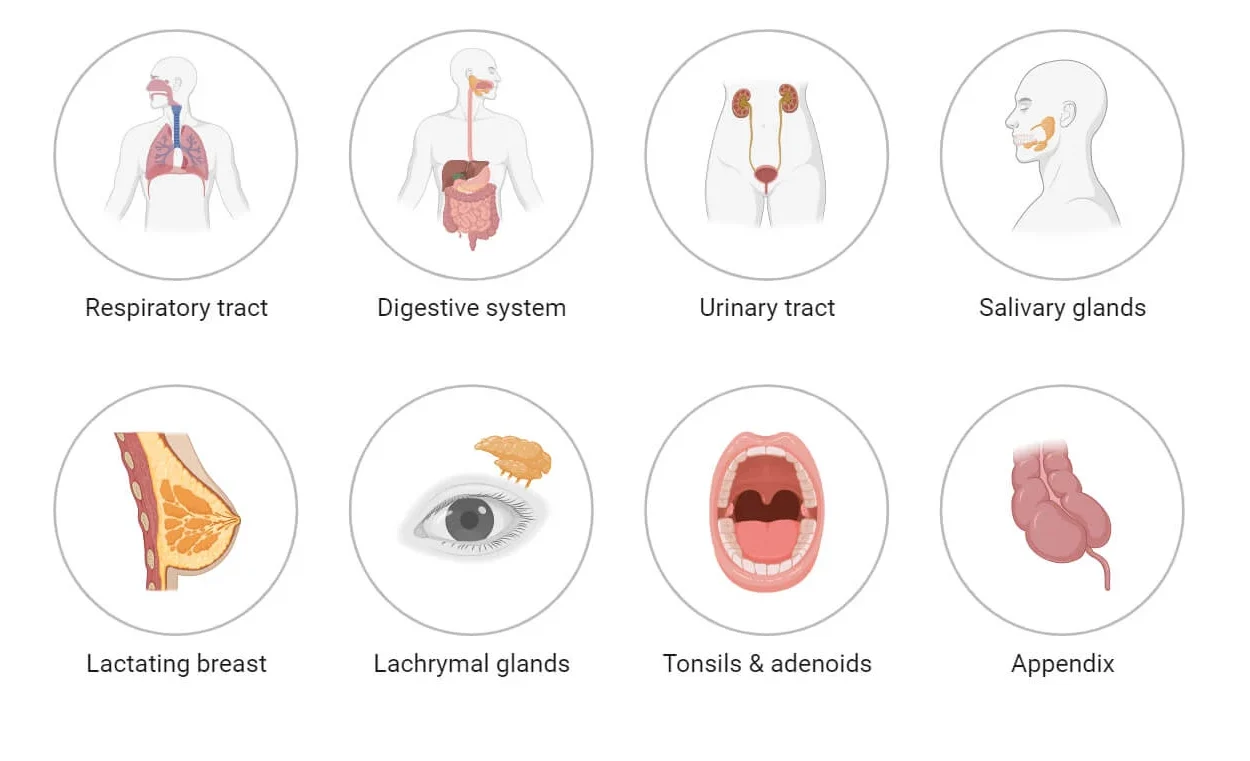
Gastrointestinal Tract:
- The entire digestive system is lined with mucous membranes, including the oral cavity (mouth), pharynx, esophagus, stomach, small intestine, and large intestine (colon). These mucosal linings aid in digestion, absorption of nutrients, and protection against pathogens.
Respiratory Tract:
- Mucous membranes line the respiratory tract, starting from the nasal cavity and extending through the trachea, bronchi, and bronchioles to the alveoli in the lungs. These membranes produce mucus to trap and remove particles, humidify and warm the air, and provide a protective barrier.
Urogenital Tract:
- The mucous membranes are present in the urinary tract, including the urethra, bladder, and parts of the ureters and kidneys. In the female reproductive system, mucosa lines the vagina and uterus. In males, it lines the urethra. These mucosal linings play roles in excretion, urine storage, and reproduction.
Oral Cavity and Salivary Glands:
- The oral cavity, including the lips, cheeks, tongue, and associated structures, is lined with mucous membranes. Salivary glands, which produce saliva to aid in digestion, also have mucosal linings.
Nasal Cavity and Paranasal Sinuses:
- The nasal cavity, responsible for breathing and olfaction, is lined with mucous membranes. The paranasal sinuses, connected to the nasal cavity, also have mucosal linings.
Conjunctiva of the Eyes:
- The conjunctiva, a mucous membrane, lines the surface of the eye and the inner surface of the eyelids. It helps keep the eye moist and protected.
Auditory Tubes and Middle Ear:
- The mucous membranes line the auditory tubes (eustachian tubes) connecting the middle ear to the nasopharynx. The middle ear is also lined with mucosal tissue.
Mouth and Esophagus:
- Beyond the oral cavity, mucous membranes continue into the esophagus, facilitating the movement of food during swallowing.

These locations highlight the diverse roles of mucous membranes in the body, ranging from facilitating digestion and respiration to providing protection and maintaining tissue integrity. Each region has specific adaptations of the mucosa to suit its functional requirements.
Functions of Mucous Membrane
Mucous membranes, or mucosa, serve several crucial functions in the body, providing a protective interface between the external environment and internal organs. The general functions of mucous membranes include:
Protection:
- Physical Barrier: The epithelial layer of mucous membranes acts as a physical barrier, preventing the entry of pathogens, toxins, and foreign particles into the body.
- Secretion of Mucus: Goblet cells in the mucosa produce mucus, a viscous fluid that helps trap and eliminate microbes, dust, and other irritants. Mucus also provides lubrication to prevent friction and damage.
Secretion and Absorption:
- Glandular Secretions: Mucosal glands, including goblet cells, release various substances such as enzymes, antibodies, and antimicrobial peptides. These secretions aid in digestion, immune defense, and maintaining a favorable environment for physiological processes.
- Selective Absorption: Mucous membranes are involved in the absorption of nutrients and water. The specific epithelial cells in different mucosal regions are adapted for the selective uptake of substances based on the needs of each organ.
Immune Defense:
- Immunoglobulin Secretion: Mucosal-associated lymphoid tissue (MALT) present in mucosal membranes produces immunoglobulins (IgA) and other immune factors. These components contribute to local and systemic immune responses, protecting against infections.
Moistening and Lubrication:
- Mucus Production: Mucous membranes produce mucus to keep surfaces moist, preventing dehydration and maintaining optimal conditions for physiological processes. This is particularly important in areas exposed to air, such as the respiratory and digestive tracts.
Sensory Functions:
- Sensory Receptors: Mucous membranes contain sensory nerve endings that detect changes in the environment. For example, taste buds in the oral mucosa contribute to the sense of taste, while sensory receptors in the nasal mucosa play a role in olfaction (sense of smell).
Facilitation of Movement:
- Smooth Muscle Function: In some mucosal regions, such as the gastrointestinal tract, the muscularis mucosae layer facilitates the movement of substances, aiding in processes like peristalsis and the propulsion of food through the digestive system.
Temperature Regulation:
- Vasodilation and Blood Flow: Mucosal blood vessels and capillaries play a role in temperature regulation. Vasodilation and changes in blood flow help adjust the temperature in response to environmental conditions.
Exchange of Gases:
- Respiratory Mucosa: In the respiratory tract, mucous membranes facilitate the exchange of gases by providing a moist surface for the diffusion of oxygen and carbon dioxide.
These functions collectively contribute to the overall health and homeostasis of the body, emphasizing the versatile roles of mucous membranes in different organ systems.
Mucosal Immunity
Mucosal Immunity, emphasizing its importance in defending the body against pathogens at mucosal surfaces. Here are some key points from your provided information:
Definition of Mucosal Immunity:
- Mucosal immunity, or mucosal-associated lymphoid tissue (MALT), is a component of the immune system that operates at mucous membrane surfaces. Its primary function is to protect the host from potential pathogens in the environment.
Mucosal Sites and Categories:
- Mucosal immunity is associated with specific mucosal sites, including the gut mucosa (Peyer’s Patches, intestinal lamina propria, cryptopatches, and lymphoid follicles). It can be categorized based on location, such as gut-associated lymphoid tissue (GALT), nasopharynx-associated lymphoid tissue (NALT), bronchus-associated lymphoid tissue (NALT), conjunctiva-associated lymphoid tissue (CALT), and lachrymal duct-associated lymphoid tissue (LDALT).
IgA Antibodies:
- Immunoglobulin A (IgA) cells are prominent in mucosal immunity. They are the most common B cells involved in the immune response at mucosal surfaces. IgA antibodies are produced and secreted by mucosal-associated lymphoid tissue (MALT), particularly in the gut mucosa.
Functions of IgA Antibodies:
- IgA antibodies play a crucial role in mucosal immunity by neutralizing food antigens, inhibiting commensal bacteria, and countering bacterial pathogens. This helps prevent the entry and colonization of harmful microorganisms in mucosal tissues.
T Cells and Regulation:
- T cells of thymic origin are involved in the regulation of mucosal immunity. They play a role in the differentiation of IgA precursors, contributing to the production of specific antibodies tailored for mucosal defense.
Neutralization and Inhibition:
- IgA antibodies contribute to the neutralization of antigens, preventing their harmful effects. This includes neutralizing food antigens and inhibiting the colonization of both commensal and pathogenic bacteria.
Overall, mucosal immunity represents a specialized defense mechanism that operates at the interfaces between the body and the external environment, safeguarding mucosal surfaces from potential threats. The presence of specific lymphoid tissues and the production of IgA antibodies are key components of this immune response.
Common disorders affecting mucous membranes
Several disorders can affect mucous membranes, leading to various symptoms and complications. Here are some common disorders that impact mucous membranes:
Oral Thrush (Candidiasis):
- Cause: Overgrowth of the Candida fungus, particularly Candida albicans.
- Symptoms: White, creamy lesions on the tongue, inner cheeks, and other oral surfaces, along with redness and discomfort.
- Treatment: Antifungal medications.
Gingivitis:
- Cause: Inflammation of the gums, often due to poor oral hygiene leading to the accumulation of plaque.
- Symptoms: Swollen, red gums that may bleed during brushing or flossing.
- Treatment: Improved oral hygiene, professional dental cleaning.
Stomatitis:
- Cause: Inflammation of the oral mucous membranes, often caused by viral infections, autoimmune conditions, or irritants.
- Symptoms: Painful sores, redness, and swelling in the mouth.
- Treatment: Depends on the underlying cause, may include antiviral medications or immune-modulating drugs.
Conjunctivitis (Pink Eye):
- Cause: Inflammation of the conjunctiva, often due to viral or bacterial infections, allergies, or irritants.
- Symptoms: Redness, itching, tearing, and discharge from the eyes.
- Treatment: Depends on the cause; may include antiviral or antibiotic eye drops, and anti-allergy medications.
Gastroesophageal Reflux Disease (GERD):
- Cause: Chronic condition where stomach acid flows back into the esophagus, causing irritation.
- Symptoms: Heartburn, regurgitation, chest pain, and irritation of the esophageal mucosa.
- Treatment: Lifestyle changes, medications to reduce stomach acid.
Inflammatory Bowel Disease (IBD):
- Types: Crohn’s disease and ulcerative colitis.
- Cause: Chronic inflammation of the gastrointestinal tract.
- Symptoms: Abdominal pain, diarrhea, rectal bleeding, and inflammation of the mucous membranes in the digestive system.
- Treatment: Medications to control inflammation, lifestyle changes, and in severe cases, surgery.
Recurrent Aphthous Stomatitis (Canker Sores):
- Cause: Not fully understood; may be related to immune system dysfunction or genetic factors.
- Symptoms: Painful, shallow sores on the inner lips, cheeks, or tongue.
- Treatment: Symptomatic relief with topical numbing agents, oral rinses, and sometimes corticosteroids.
Lichen Planus:
- Cause: Chronic inflammatory condition of the skin and mucous membranes.
- Symptoms: White, lacy patches on the oral mucosa, along with skin lesions.
- Treatment: Topical or systemic corticosteroids, depending on the severity.
It’s essential to seek medical attention for persistent or severe symptoms related to mucous membrane disorders, as appropriate diagnosis and treatment are crucial for managing these conditions effectively.
Maintaining mucosal health
Maintaining mucosal health is vital for overall well-being, as mucous membranes play a crucial role in protecting the body from external threats and facilitating various physiological functions. Here are some key aspects and practices to promote mucosal health:
Hydration:
- Importance: Proper hydration is essential for maintaining mucous membrane moisture. Well-hydrated mucous membranes are more effective at trapping and eliminating pathogens.
- Recommendation: Drink an adequate amount of water throughout the day to support overall hydration.
Good Oral Hygiene:
- Importance: Oral mucosa is susceptible to various infections and irritations. Good oral hygiene practices help prevent conditions such as gingivitis and oral thrush.
- Recommendation: Brush teeth regularly, floss, and use mouthwash to maintain oral health. Regular dental check-ups are also important.
Balanced Nutrition:
- Importance: Proper nutrition supports the immune system and contributes to the health of mucous membranes. Nutrient deficiencies can compromise mucosal integrity.
- Recommendation: Consume a balanced diet rich in vitamins, minerals, and antioxidants. Include fruits, vegetables, whole grains, and lean proteins.
Avoidance of Irritants:
- Importance: Exposure to irritants can damage mucous membranes, leading to inflammation and increased susceptibility to infections.
- Recommendation: Minimize exposure to smoke, pollutants, allergens, and other irritants. Use protective measures when necessary.
Regular Exercise:
- Importance: Physical activity contributes to overall immune function and can positively impact mucosal health.
- Recommendation: Engage in regular exercise as part of a healthy lifestyle.
Stress Management:
- Importance: Chronic stress can weaken the immune system and impact mucosal health. Stress management is crucial for overall well-being.
- Recommendation: Practice stress-reducing techniques such as meditation, deep breathing, yoga, or other relaxation methods.
Adequate Sleep:
- Importance: Sleep is essential for immune system function and tissue repair, including mucosal tissues.
- Recommendation: Aim for 7-9 hours of quality sleep each night.
Probiotics:
- Importance: Probiotics, beneficial bacteria, play a role in maintaining a healthy balance of microorganisms in the mucosa, particularly in the digestive system.
- Recommendation: Consume probiotic-rich foods or supplements to support gut health.
Regular Health Check-ups:
- Importance: Regular medical check-ups can help identify and address potential mucosal health issues early on.
- Recommendation: Schedule regular health check-ups with healthcare professionals for preventive care.
Personal Hygiene:
- Importance: Proper personal hygiene practices help prevent infections that can affect mucous membranes, particularly in the genital and urinary tract.
- Recommendation: Follow good personal hygiene practices, including regular handwashing.
Maintaining mucosal health is an integral part of a holistic approach to overall health and immunity. Healthy lifestyle choices contribute to the resilience of mucous membranes and their ability to fulfill their protective functions.
Comparison
with Serous Membranes:
| Character | Mucous membrane | Cutaneous membrane |
| Location | Found lining body cavities that open to the external environment, such as the digestive, respiratory, and reproductive tracts. | Line closed body cavities, such as the thoracic and abdominal cavities, and cover organs within these cavities. |
| Secretion | Produce mucus, a lubricating and protective fluid. | Produce serous fluid, which lubricates and reduces friction between organ surfaces. |
| Protection | Primarily protect against pathogens and facilitate the movement of materials. | Primarily protect against friction and abrasion between organs and body cavities. |
| Function | Involved in absorption, secretion, and protection at interfaces with external environments. | Facilitate organ movement, protect against friction, and help maintain organ position. |
| Epithelial Layer | Typically stratified squamous or simple columnar epithelium. | Composed of simple squamous epithelium. |
with Cutaneous (Skin) Tissues:
| Character | Mucous membrane | Cutaneous membrane |
| Location | Found internally lining body cavities open to the external environment. | Covers the external surface of the body. |
| Secretion | Produce mucus for lubrication and protection. | Produce sweat and sebum for thermoregulation and protection. |
| Protection | Primarily protect against pathogens and facilitate material exchange. | Protect against physical damage, pathogens, and dehydration. |
| Function | Involved in absorption, secretion, and protection at interfaces with external environments. | Primary barrier against external threats, regulates temperature, and houses sensory receptors. |
| Epithelial Layer | Typically stratified squamous or simple columnar epithelium. | Composed of stratified squamous epithelium. |
Commonalities:
- Both mucous membranes and cutaneous tissues serve protective functions.
- Both have an epithelial layer, but the specific types of epithelia may vary.
- Both involve the production of secretions (mucus in mucous membranes, sweat, and sebum in cutaneous tissues).
- Both are exposed to environmental factors and play roles in maintaining homeostasis.
Differences:
- Mucous membranes are found internally, lining body cavities open to the external environment, while cutaneous tissues are external and cover the body surface.
- Mucous membranes primarily protect against pathogens and facilitate material exchange, while cutaneous tissues protect against physical damage, pathogens, and dehydration and also regulate temperature.
- The types of secretions and the specific functions differ between mucous membranes and cutaneous tissues.